What is Bone Marrow Transplant ?
The tissue inside the bones known as bone marrow includes blood-forming cells known as Hematopoietic Stem Cells (HSC). If the bone marrow malfunctions due to factors such as cancer (Leukemia), Thalassemia, or immunological causes (Aplastic Anemia), a deficit of produced blood components develops, resulting in weakness, infections, and bleeding, finally leading to death. A bone marrow or hematopoietic stem cell transplant is a surgical operation that replaces diseased marrow with healthy marrow or hematopoietic stem cells. A bone marrow transplant is a critical treatment that can save a person's life. The body's functionality deteriorates due to a lack of fresh blood cells. As a result, rapid transplantation is required for people to regain their lost physical functions and strength.

Why do you need Bone Marrow Transplant ?
Traditional treatment options for some diseases, such as Thalassemia, are primarily supportive blood / component transfusions requiring multiple blood donors and frequent hospitalisation, ultimately resulting in iron overload, organ toxicities, growth failure, and viral (HIV, Hepatitis B, Hepatitis C) infections. Allogenic bone marrow / stem cell transplantation is the sole curative option for these patients.
Similarly, Chemotherapy was used to
treat leukaemia, but allogenic transplant remains the most potent anti-leukemia
therapy and is a curative possibility. The principle of leukaemia treatment is
that the higher the dose, the better the disease control. Due to the deadly
toxicity of bone marrow loss, very high dosages of chemotherapy cannot be
administered. During the transplant, a strong dosage of chemotherapy is used to
kill the diseased bone marrow, but this is followed by the infusion of donor's
hematopoietic stem cells (allogenic transplant) or the patient's own
pre-collected stem cells (autologous transplant) to restore blood production.
Diseases in which Bone Marrow Transplant is Recommended ?
Aplastic Anemia and other bone marrow failure syndromes:
These disorders are life-threatening and are characterised by the failure of the bone marrow to create adequate blood components to meet the needs of the patients. Patients with low haemoglobin, leucocytes, and platelets typically require blood and platelet transfusions. For such individuals, a timely Allogeneic stem cell transplantation could save their lives.
- Thalassemia Major:
- This is a hereditary illness in which a child requires
regular blood transfusions since infancy due to a haemoglobin genetic
abnormality. Without proper blood transfusions and iron chelation
medication, this is a potentially fatal condition. Most thalassemia
patients can be cured with an allogeneic stem cell transplant while they
are young.
Sickle Cell Anemia:
This is another inherited haemoglobin condition that produces
severe episodes, stroke, and organ failure in addition to anaemia. Most of
these patients can be cured with an allogeneic stem cell transplant.
Hemophagocytic Syndrome:
This is a devastating condition that can be fatal in a
matter of minutes and can be cured with an allogeneic stem cell transplant.
There are numerous more conditions where a stem cell transplant can save a person's life, such as inborn metabolic defects, congenital immunodeficiency syndromes, and so on.
Multiple Myeloma (MM): This is a plasma cell cancer that can cause anaemia, kidney dysfunction, bone disease, infections, and can be fatal if not treated early. Chemotherapy and autologous stem cell transplantation are used to treat Multiple Myeloma. Autosomal stem cell transplantation may improve these patients' chances of survival.
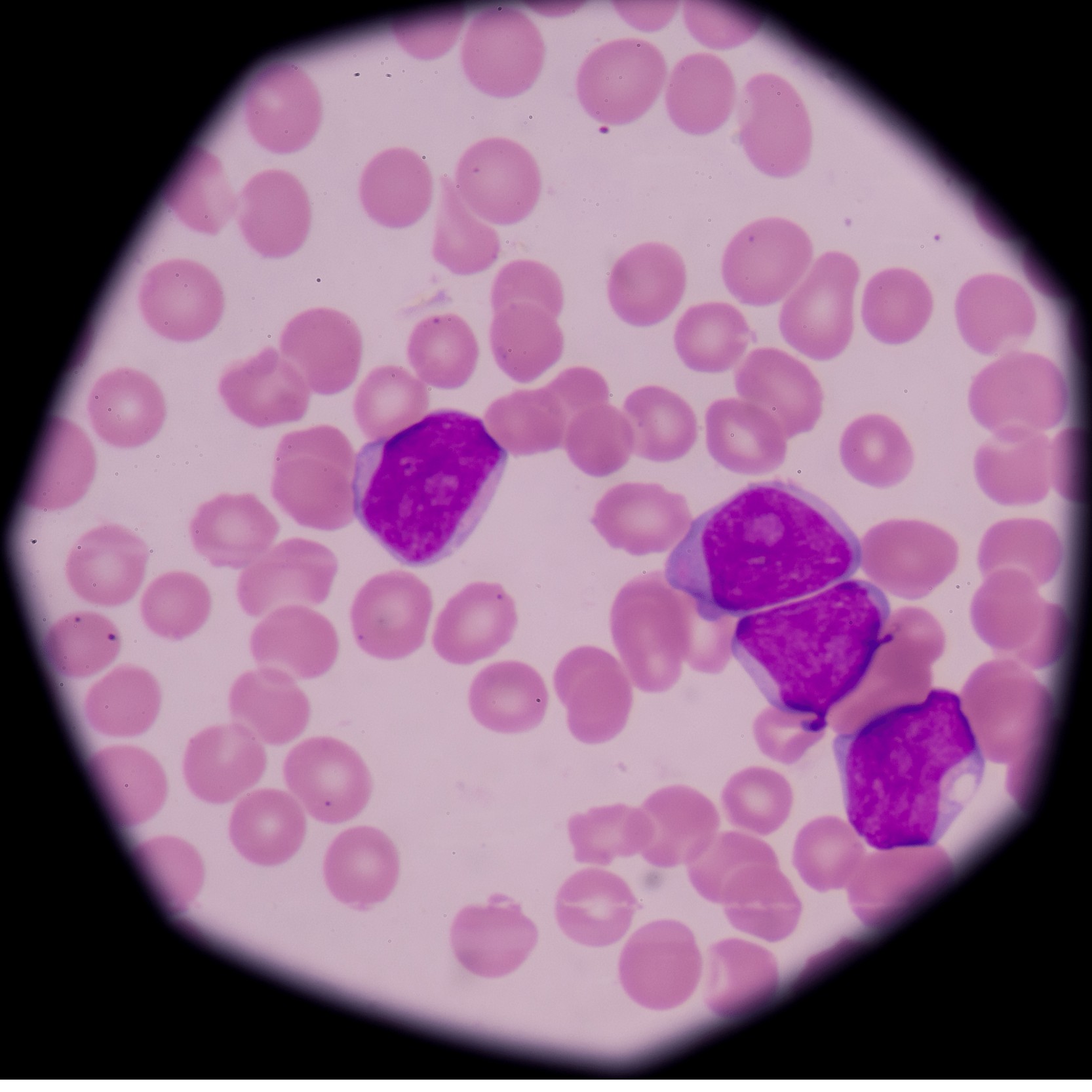
Acute Myeloid Leukemia (AML): This is an aggressive blood cancer that can be fatal. To establish a cure, moderate to high risk AML requires extensive chemotherapy as well as Allogeneic Stem Cell Transplantation
Acute Lymphoblastic Leukemia (ALL): This is another aggressive and potentially fatal blood cancer that is mainly treated with chemotherapy. Few high-risk ALL patients, as well as those who have relapsed despite chemotherapy, require Allogeneic stem cell transplantation to be cured
Chronic Myeloid Leukemia (CML): The majority of CML patients are treated with targeted medicines. Only a few individuals who do not respond well to targeted medications are treated with Allogeneic Stem Cell Transplantation in order to be cured.
Myelofibrosis, Myelodysplastic syndrome (MDS), Chronic Myelo-Monocytic Leukemia (CMML), and other similar blood cancers: Allogeneic stem cell transplantation is used to cure these blood cancers. Certain people may require chemotherapy before receiving a transplant.
Sources of hematopoietic stem cells
Bone Marrow:
Bone Marrow stem cells are
collected using aspiration needles from the iliac crest (hip bone). It is
performed under general anaesthesia, is painless, and the donor is discharged
the next day. In disorders such as Thalassemia or Aplastic Anemia, bone marrow
stem cells are preferred. When using bone marrow as a graft source, the
recovery period is longer than when using peripheral blood stem cells, but the
risk of graft against host disease is lower.
Peripheral Blood:
Stem cells can also be
extracted from bigger veins of the body using an apheresis procedure using a
cell separator machine after 4-5 days of growth factor injections. It is a very
safe and dependable operation that takes only a few hours and requires no
anaesthesia. With plerixafor and G CSF support, even difficult-to-mobilize
patients can have their stem cells extracted. Recovery from a peripheral blood
stem cell graft is 5-7 days faster than from a bone marrow graft. This type of
transplant is preferable for patients with leukaemia, myeloma, or lymphoma.
Cord Blood:
Blood obtained from the placenta following birth is a strong source of Hematopoietic Stem Cells and can also be used for allogenic stem cell transplants. The issue is a lack of volume and cell dosage, which causes delayed recovery and engraftment failure.
Types of Bone Marrow Transplant
Autologous stem cell transplantation (ASCT):
Stem Cells are extracted from the patient's own blood. ASCT, as it is mostly used to treat patients with Multiple Myeloma, Lymphomas, and Neuroblastoma.
Allogeneic stem cell transplant:
In this procedure, stem cells are obtained from a healthy donor. The donor is frequently a family member who matches the patient's HLA (Tissue antigens). There are various donor categories depending on the donor's link to the patient and the degree of HLA match:
Fully HLA matched related (family) donor
Fully HLA matched unrelated donor
Half match related donor (Haplo-identical donor)
The use of a
patient's own Hematopoietic Stem Cells is referred to as autologous transplant.
It is typically used to treat multiple myeloma, relapsed Hodgkin and
non-Hodgkin lymphoma, and T lymphoma. After establishing at least a partial
response in disease, a patient's stem cells are collected, and then a very high
dose of Chemotherapy is administered to destroy existing disease, followed by
reinfusion of collected stem cells to reestablish blood formation.
Stem cells are collected from a healthy donor in an allogenic transplant. This healthy donor is usually a sibling (related donor fully matched or haploidentical), but it can also be received from an international donor registry (unrelated donor) or from umbilical cord blood. Voluntary donor registries in India, like as DATRI, are extremely active and have provided donors for numerous transplants.
Bone Marrow Transplant Procedure
- Stem cell collection from a donor or patient, conditioning with chemo-radiotherapy for the patient, stem cell infusion, pre-engraftment bone marrow suppression, and post-engraftment follow up are all part of the transplant process. In the BMT unit, the average period before engraftment is 3-4 weeks. Following that, the patient is sent home on oral drugs to avoid graft against host illness and infections. For the first 3-6 months after transplant, patients must be closely monitored and recommended to stay nearby to the Hospital. By one year after the transplant, the patient's immune system has recovered and most medications can be discontinued.
Stem Cell Collection: Stem cells are extracted from
donors' blood (in allogeneic transplants) using a cell separator machine or by
aspirating bone marrow. In an autologous transplant, stem cells are extracted
from the patient's blood using a cell separator machine. As a result, it can
only be done when the disease has been controlled with regular treatment.
Conditioning: Conditioning refers to the use of
high-dose Chemotherapy or Radiotherapy to destroy or inhibit the patient's
existing bone marrow and cause immunosuppression so that donor stem cells can
home in and begin functioning. The drugs used in conditioning vary depending on
the underlying illness for which the transplant is performed.
Stem Cell Infusion & Engraftment: Similar to blood transfusion, Stem Cells or Bone Marrow are delivered to the patient through veins after conditioning. These stem cells subsequently travel to the bone marrow, where they settle and begin making blood cells. The time it takes for blood to be produced is referred to as the engraftment period. Patients' blood counts are considerably low for 10-20 days prior to engraftment, and the risk of infection is considerable, hence patients are maintained in strict isolation and hepa-filtered rooms. During this time, the patient will require frequent blood/platelet transfusions as well as continuous monitoring of blood counts.
Side effects of transplant are caused by chemo/radiotherapy used in conditioning, which is seen in both autologous and allogenic transplants, or by an immunological reaction known as graft versus host disease, which is seen in allogenic transplants.
Nausea,
Vomiting, and Loss of Appetite — These symptoms usually last a few days. With
the availability of modern medications, it is possible to avoid and control it
to a large extent.
Mouth Ulcers
- These are usually small, only last a few days, and do not require any
treatment other than pain relief. When the condition is severe enough to
prevent patients from drinking or swallowing, they are given nutrients through
veins.
Hair Loss — Hair loss is caused
by high-dose chemotherapy or radiotherapy used in conditioning, but it is only
temporary because hairs grow back within a few months after transplant.
Fever -
Patients are prone to infections due to significantly low white blood cell
counts before to engraftment. Patients are maintained in strict isolation rooms
with filtered air to avoid infection until their blood counts improve.
Platelets are the blood component
that prevents bleeding, and their count dropped after conditioning, increasing
the risk of bleeding in the skin, mouth, nose, or other areas. Platelets are
transfused to maintain an adequate platelet count in order to prevent
haemorrhage. When engraftment occurs, platelet production begins and the risk
of bleeding vanishes.
Fertility — Due to the side
effects of chemotherapy and radiotherapy, practically all adult and adolescent
male and female patients may have temporary or permanent sterility following
transplant, despite the fact that the ability to have sex is not affected by
transplant. It is recommended that male patients who intend to have children
have their sperm saved for future use.
Graft Versus Host Disease - Graft
Versus Host Disease is a side effect of Allogenic Transplantation that arises
after engraftment (GVHD). It refers to the reaction of a donor's blood cell to
the patient's body. It happens despite the fact that the patient and donor are
HLA matched, thus medications are provided to avoid it. It is typically mild,
affecting the skin (rashes), liver (jaundice), or intestines (loose movements,
abdominal pain), but it can be serious and life threatening in a small
percentage of people. The presence of GVHD does not imply that the transplant
has failed. This can be effectively treated with immunosuppressive treatments.
Relapse - Even if the transplant is performed with the intention of curing the patient, certain individuals with aggressive disease may relapse. After two years, the likelihood of relapse is greatly reduced. Many patients can be saved from relapse by periodically monitoring the patient for relapse and intervening early with chemotherapy, lowering immune suppression, or donor lymphocyte infusion.
Einstagore helpdesk
Please contact us on :
+91 95 99 88 1050
