What is Sickle-cell disease Anaemia ?
Sickle-cell disease
Anaemia, also known as Sickle cell disease, is a genetically inherited form of
anaemia that is most frequent in people of African, Arabian, and Indian
descent. It is a condition in which the body is unable to create enough red
blood cells to deliver enough oxygen throughout the body. This can result in a
stroke, acute chest syndrome, pulmonary hypertension, organ damage, blindness,
gallstones, and other consequences. While there is no permanent cure for this
disease, some treatment regimens can assist prevent any consequences that may
occur as a result of it.
Causes of Sickle Cell Disease
A mutation in the gene that produces haemoglobin, the iron-rich
substance found in red blood cells that gives blood its red colour, causes
sickle cell disease.
The
major type of haemoglobin in healthy people without sickle cell anaemia is HbA,
which allows red blood cells to transport oxygen from the lungs to all regions
of the body.
Symptoms
Sickle cell anaemia symptoms can vary from person to person and alter over time. The majority of the symptoms are caused by the haemolysis and occlusion that occurs along the course of the disease. Typical symptoms include:
Fatigue caused by anaemia: Normal red blood cells function for 120 days before being replaced. Sickle-shaped red blood cells, on the other hand, are readily destroyed within 10 to 20 days and so impair oxygen circulation in the body. This causes chronic weariness as well as other concerns such as shortness of breath, fainting spells, and so on.
Hand and foot inflammation: Painful
swelling of the hands and feet is caused by sickle-shaped red blood cells that
tend to obstruct blood flow to the extremities, particularly the hands and
feet.
Frequent Infections: Sickle-shaped red blood cells harm the spleen, which is in charge of recycling red blood cells as well as storing platelets and white blood cells. As a result, the immune system is weakened, and the body is more vulnerable to infections.
Periodic episodes of pain: 'Crises,' or periodic
episodes of pain, occur when sickle-shaped red blood cells obstruct blood flow.
Pain is felt in the muscles, bones, joints, chest, and other areas, and it might
linger for several hours.
Impaired growth/development: Red blood
cells are in charge of the body's oxygen and nutrition delivery. Growth and
development are hampered by a lack of red blood cells caused by sickle cell
disease.
Impaired vision: Sickle-shaped red blood cells can sometimes obstruct the tiny blood arteries of the eye, causing significant damage to the retina and, as a result, visual impairment.
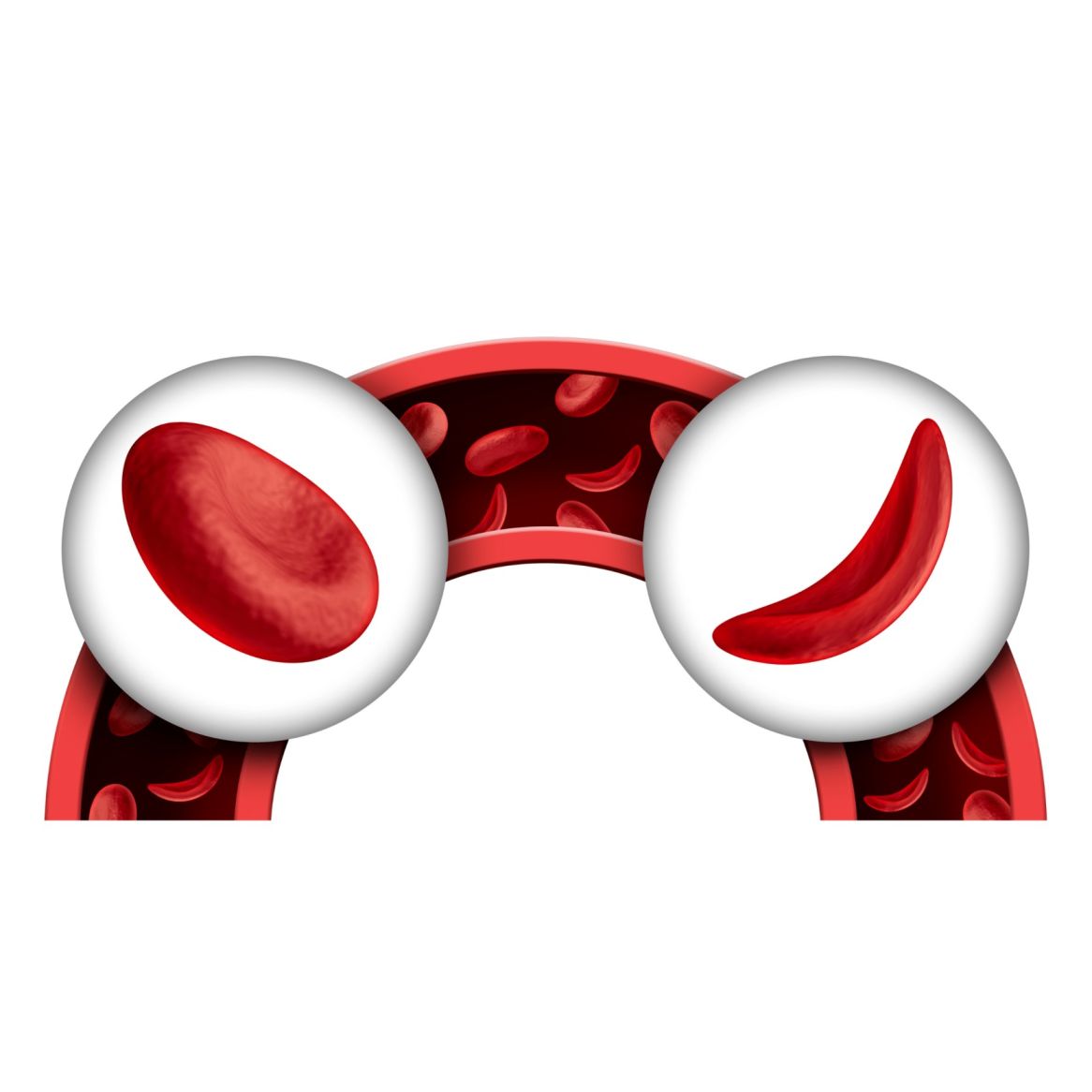
Genealogy of the disease
The sickle-cell anaemia gene is passed down from generation to generation in a genetic pattern known as Autosomal-Recessive Inheritance. This means that for the kid to be impacted with the disease, both parents must be 'carriers,' and both mother and father must pass on the defective gene. When only one parent is a carrier, the kid may receive 'the sickle cell trait' from that parent, becoming a carrier with one faulty haemoglobin gene (HbS) and one normal haemoglobin gene (HbA). Carriers or those with sickle-cell trait do not experience sickle-cell anaemia symptoms. Their blood, on the other hand, will contain both typical biconcave and sickle-shaped red blood cells.
Sickle
cell Anaemia Treatment
Treatment for sickle cell anaemia is typically targeted at
alleviating symptoms and preventing complications. Anyone suffering from this
disease must have their red blood cell count and health checked, which is why
regular check-ups with a licenced doctor are critical. The following are some
popular treatments for sickle cell anaemia symptoms:
Medication: Medications
used to treat sickle-cell anaemia include:
1. Antibiotics: Children
with sickle cell anaemia may be given antibiotics such as penicillin as early
as 2 months of age and may continue to take the medications until they are 5
years old. Antibiotics aid in the prevention of potentially fatal illnesses
such as pneumonia and jaundice. Adults might also be given these antibiotics as
a prophylactic precaution against certain infections.
2. Pain relievers: People
suffering from Crises or recurring episodes of pain, which is one of the most
noticeable symptoms of Sickle cell anaemia, may be given pain relievers.
3. Hydroxyurea: It can be used on a daily basis to reduce discomfort caused by crises. This medication has been shown to increase the body's production of foetal haemoglobin, a kind of haemoglobin seen in infants that helps prevent the formation of sickle cells. Long-term usage of hydroxyurea, on the other hand, may result in certain serious side effects. As a result, it is critical to consult a doctor before taking this medication and to use it only as advised by a licenced healthcare expert and doctor.
Blood Transfusions: Regular blood
transfusions help to maintain the red blood cell count under control, allowing
the symptoms of anaemia to be managed. People who have sickle cell anaemia are
at a higher risk of having a stroke. Blood transfusions can also help to reduce
this danger and so extend a patient's life.
Vaccinations: Sickle-cell anaemia
weakens the immune system, making the patient more vulnerable to diseases.
Childhood vaccines help reduce the chance of developing life-threatening
diseases, especially in children with sickle cell anemia
Supplemental Oxygen: Adding
oxygen to the blood and improving circulation are two benefits of using supplemental
oxygen through a breathing mask. It is especially beneficial when the patient
has acute chest syndrome or a sickle-cell crisis.
Bone marrow transplant: The bone marrow is the primary source of red blood cells. As a result, a bone marrow transplant is the most effective means of treating sickle-cell anaemia, in which the patient's impacted, sickle-cell generating bone marrow is replaced with healthy bone marrow that generates normal red blood cells.
Bone marrow transplantation is a viable and promising treatment option for haematological illnesses such as sickle cell anaemia. The faulty bone marrow is replaced with healthy bone marrow transplanted from a matching donor in this approach. As a result, the new healthy bone marrow will create healthy and efficiently functioning red blood cells rather than the sickle-shaped red blood cells that were initially produced by the patient's bone marrow.
Finding an appropriate donor for the transplantation candidate is one of the most crucial aspects of the process. The treatment process begins with tests to see if the donor and patient have a tissue match. The doctor removes healthy cells from the donor's bone marrow and injects them into the patient's body via an IV tube during this procedure. When the injected cells continue to operate normally in the recipient's body, it is declared to be a match, and the bone marrow transplant is performed after a few more comparable tests.
Bone marrow transplants are the only viable solution for sickle cell disease in India. This approach is highly effective in around 90% of cases involving youngsters with the disease. Certain medications must be taken to reduce the chance of rejection of the transplanted bone marrow.
